Background:
Newly diagnosed Multiple Myeloma (MM) patients have a 10 to 20 times higher risk of developing venous thromboembolism (VTE) than the general population. The pathogenesis may involve several factors such as activation of procoagulant factors, acquired activated protein C resistance, and inflammation. In addition to the general risk factors for venous thromboembolism such as older age, immobility, and surgery, some MM treatment-related factors such as the use of immunomodulatory drug therapy and abnormal cytogenetics contribute to the increased risk. The PRISM score (Prior VTE, Race, IMiD, Surgery, Metaphase Cytogenetics) is a risk prediction tool for VTE in MM and was published in 2022. The score ranges from 0 to 18 and patients were stratified into three groups: low (0), intermediate (1-6), and high risk (≥ 7). Our primary objective was to assess the external validity of the PRISM score in our community hospital setting.
Methods:
All consecutive newly diagnosed MM treated at Saint Vincent Hospital from 1/1/2008 to 12/22/2022 were included in our analysis. Patients receiving therapeutic anticoagulation for other indications or a diagnosis of VTE within 6 months preceding the MM diagnosis were excluded. Variables were collected through a retrospective chart review during MM treatment initiation. Model discrimination was assessed by calculating the area under the receiver operating characteristic curve (AUROC). Logistic regression was used to calculate the odds ratio (OR) of VTE occurrence in the risk prediction model.
Results:
A total of 214 patients with newly diagnosed MM and available data on VTE occurrence were included. The median age of our cohort at treatment initiation was 74 years (range 31- 96). The median BMI was 27.8. 56% were male, and 44% were female. The mean PRISM score was 2.9, and 73% of MM were IgG/IgA subtype. IMiD-based induction regimen was used in 63 % of patients. A total of 24 patients (11.2%) were diagnosed with VTE after treatment initiation, of which 8 (3.7%) patients had a previous history of VTE. Prophylactic aspirin was used in 53.8% and abnormal metaphase cytogenetics was identified in 13% of MM cases. The median time to VTE from induction therapy was 4.8 months. The PRISM score was low in 116 patients, intermediate in 89, and high in 9 patients.
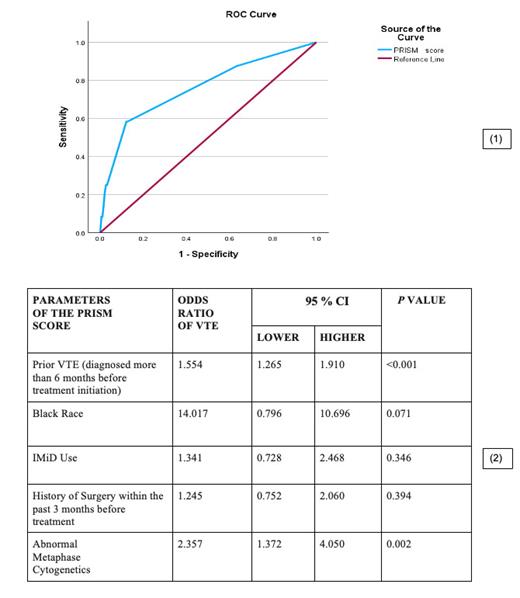
The AUROC of the model was 0.759 (95% CI, 0.644-0.874) (1). The cumulative incidence of VTE at 6 months, 12 months, and more than 1 year was 6%, 7%, and 11.2% of the patients respectively. Each 1-point increase in the score was associated with a significantly higher chance of VTE occurrence in the model [ HR= 1.53, 95% CI (1.27-1.85), P<0.001]. Among the parameters, patients with a history of VTE [ HR= 1.55, 95% CI (1.26-1.91), P<0.001] and with abnormal metaphase cytogenetics [HR= 2.35, 95% CI (1.37-4.05), P<0.001] had a higher strength of association with the development of VTE after induction (2). Furthermore, among 9 patients with a high-risk PRISM score (≥ 7), 7 (77%) developed VTE within the first 6 months after treatment initiation.
Conclusions:
Our findings suggest that PRISM [AUROC=0.75, 95% CI (0.644-0.874), P<0.001] score could statistically predict VTE outcomes in our patient population. Abnormal metaphase cytogenetics was a significant predictor of VTE in the validation cohort. Abnormal cytogenetics has been well established to be an indicator of aggressive tumor biology and proliferation in stroma-independent MM. It has been established to be a predictor of VTE in acute myeloid leukemia as well. Also, high-risk scores were predictive of earlier development of VTE after treatment induction. Our study strengthens the evidence of using PRISM as a predictive tool. Further studies are needed to enhance the sensitivity of our existing tool.
Disclosures
No relevant conflicts of interest to declare.